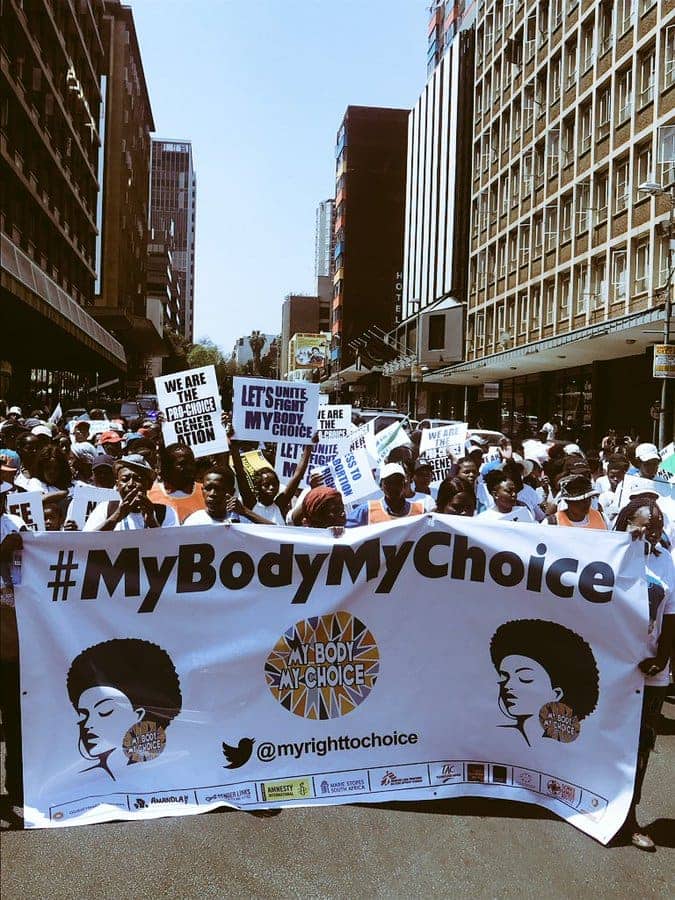
Ten years later: The NHI must prioritise sexual and reproductive health
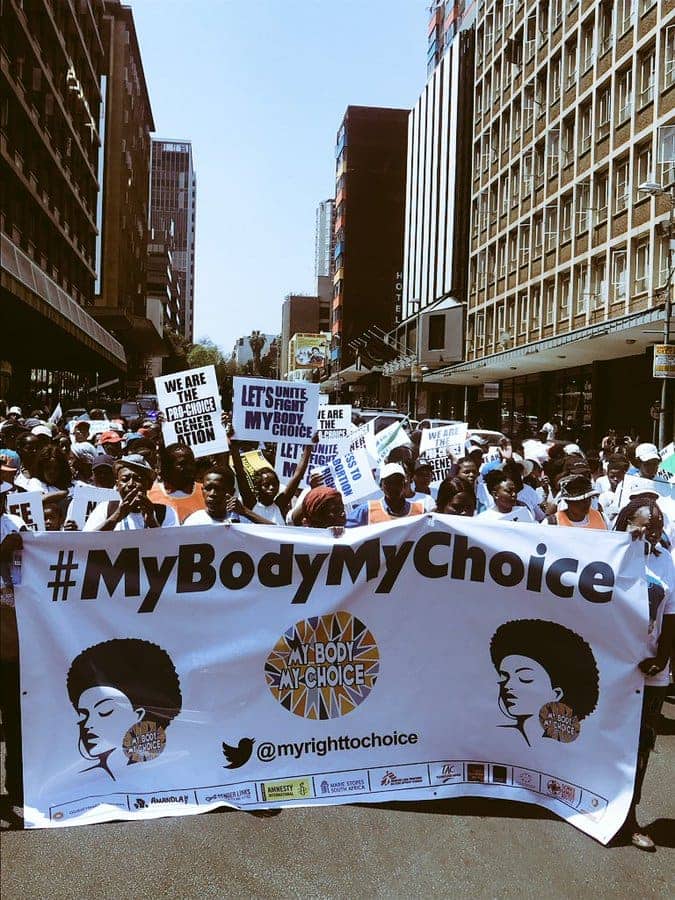
Reproductive justice is a win-win situation where everyone benefits and a South Africa universal health coverage funding model should ensure this, writes Marion Stevens.
Ten years ago, I wrote a column in the nurses’ trade union journal (Denosa Nurses Update) unpacking the National Health Insurance (NHI) and what it means for sexual and reproductive health. In writing a take two, it’s clear SA’s health system is still struggling and we need to address the inequalities.
The NHI is a funding mechanism through which our health system will deliver universal health coverage. But the current health system and the manner in which it provides for our health is not sustainable — corruption continues to plague the public and private sectors.
We’re also beholden to donors, mostly US donors representing public and private foundations, who gag and prescribe what health services can be provided in a research project or clinic – and these services are often at odds with South Africa’s legal and policy frameworks. For instance, the Gates Foundation will fund “family planning”, but will have nothing to do with abortion. As such, health services don’t talk to each other.
Gag rule influence
It’s only recently, with the reimposition of a harsher US government gag rule through the Trump administration, that donors have responded and now it’s in vogue to fund sexual and reproductive health and rights. Non-governmental organisations (NGOs) that would never have done work that involves abortion and removed themselves from civil society coalitions that promote access to abortion services 10 years ago, are now back in the circle, talking intersectionality.
International NGOs are streaming into South Africa with well-funded programmes and consultants undermining local responses. The Helms Amendment stood firm during the Obama administration. It was passed in the US Congress in 1973 and limits the use of US foreign aid for abortion. This despite advocacy groups fighting for the removal of the amendment that women in conflict situations couldn’t be funded with US government money to terminate a pregnancy that resulted from rape.
Private healthcare also guilty
How the pot of NHI funds is distributed in relation to sexual and reproductive justice will be crucial to monitor as these decisions are often political and not based on health economics or rational reasoning. Women have borne the costs of illnesses as they are squeezed out of the public sector through long queues, stock-outs, medical savings that have run out and the anti-competitive behaviour of medical aid schemes.
The influence of medical aid schemes, big pharma, international NGOs and donors has been detrimental to our health system and the nation’s health.
For those in the private sector, costs are prohibitive, with the few who are on medical aid running out of savings in March each year and having to pay out of pocket for medications. We have a culture of oversupply: pap smears are done unnecessarily for women who are not at risk of cervical cancer.
There are endless struggles around what is covered as a prescribed minimum benefit and what’s not. Why does the private sector not cover contraceptives as a prescribed minimum benefit option, while poor quality contraceptives are available mostly in the public sector? About one in five clinics across SA have contraceptive stock-outs, according to data from the national health department’s sexual and reproductive health and rights task team.
Those in the public sector have grown used to poor cover.
Low expectations for state healthcare
The public sector treats tuberculosis and has been registering new drugs to keep up with science and treatment needs. Similarly, the drugs needed to treat a sexually transmitted infection are well covered in the public sector.
Patients who go to the private sector for privacy to treat a genital discharge may just be given penicillin and not have the correct treatment given to them for the specific sexually transmitted disease they have.
The public sector has introduced cervical cancer immunisation. This treats cervical cancers but not genital warts – there are two kinds of vaccines and the government opted for the cheaper one, while the private sector provides the comprehensive option. This means cervical cancer should be less of a challenge in the future. But will boys also be included now in the vaccination campaign under the NHI as in the UK?
The regulation of funding for our health system through the National Health Insurance and the planning of universal healthcare has to be the impetus for regulation to improve, training to improve, supplies to improve and the rooting out of corruption.– Health-e News
Marion Stevens is the director of the Sexual Reproductive Justice Coalition.
An edited version of this story was published on the Daily Maverick.